By Richard Cowan and Susan Cornwell
WASHINGTON (Reuters) – The Republican-led U.S. Congress began its first session of the Donald Trump era in turmoil on Tuesday as the House of Representatives backed away from a decision to defang an ethics watchdog after a public outcry, including a dressing-down from the president-elect.
With Trump set to be sworn in as president on Jan. 20, Republicans will control both the White House and Congress for the first time since 2007, and they were set to begin laying plans for enacting his agenda of cutting taxes, repealing Obamacare and rolling back financial and environmental regulations.
But the moment was overshadowed by a surprise move by Republicans in the House of Representatives in a closed-door meeting late on Monday to weaken the independent Office of Congressional Ethics, which is in charge of investigating ethics accusations against lawmakers.
Trump, who campaigned on a pledge to “drain the swamp” and bring ethics reforms to Washington, was not pleased.
“With all that Congress has to work on, do they really have to make the weakening of the Independent Ethics Watchdog, as unfair as it may be, their number one act and priority,” he said on Twitter on Tuesday.
“Focus on tax reform, healthcare and so many other things of far greater importance!”
The ethics office was created in 2008 following several corruption scandals but some lawmakers have charged in recent years that it has been too quick to investigate complaints from outside partisan groups.
Lawmakers wanted to have greater control of the watchdog, and inserted changes into a broader rules package, set to pass when the House convenes on Tuesday.
Even before Trump’s tweet, many House Republicans, including top leaders, opposed the measure and worried about its ramifications. Trump’s tweet prompted an emergency meeting and a quick change of course by Republicans.
“It was taken out by unanimous consent … and the House Ethics Committee will now examine those issues,” said AshLee Strong, a spokeswoman for House Speaker Paul Ryan.
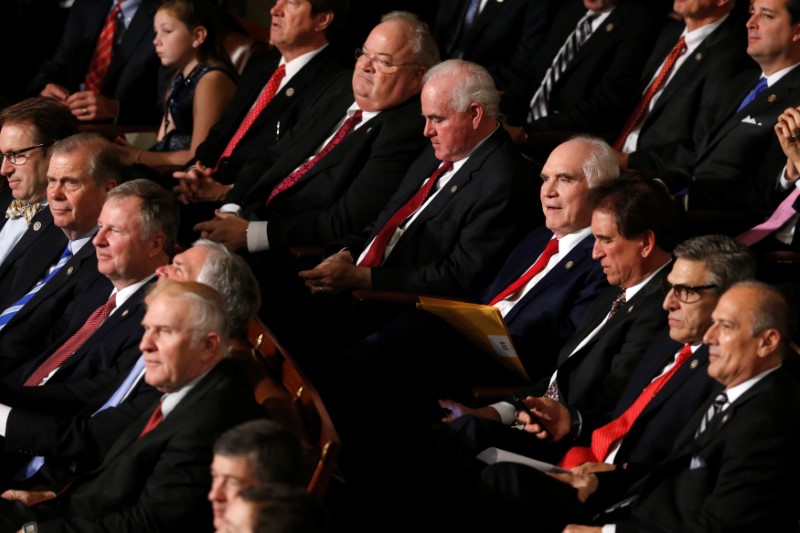
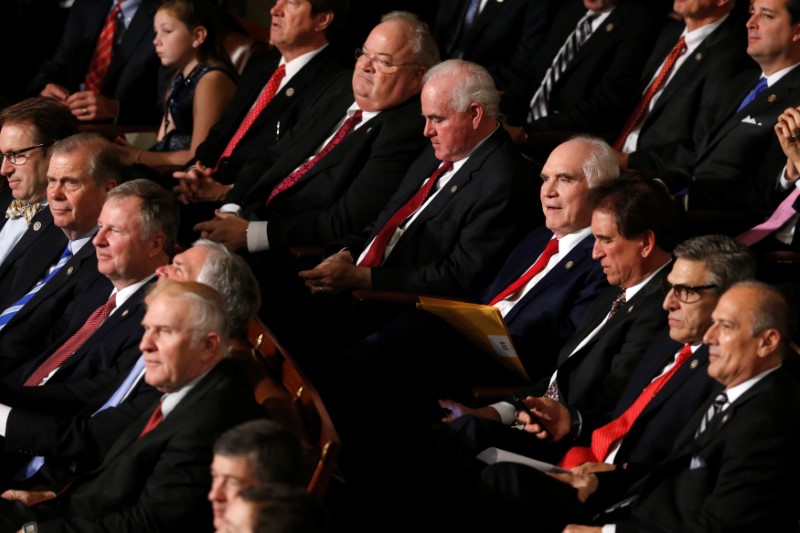
Republican members of Congress watch as they and their fellow members vote for House Speaker on the first day of the new congressional session in the House chamber at the U.S. Capitol in Washington, U.S. January 3, 2017. REUTERS/Jonathan Ernst
OBAMACARE IN SIGHTS
Since his election on Nov. 8, Trump has made clear he wants to move swiftly to enact proposals he outlined during the campaign such as simplifying the tax code, slashing corporate tax rates and repealing and replacing Obama’s signature health insurance program known as Obamacare.
Republicans have long sought to dismantle Obamacare, insisting it was unworkable and hampered job growth. But they face a dilemma over how to provide health insurance for the 13.8 million people enrolled in Obamacare who could lose their coverage. The law aims to provide health insurance to economically disadvantaged people and expand coverage for others.
Trump kept up his attack on Tuesday, tweeting: “People must remember that ObamaCare just doesn’t work, and it is not affordable,” and adding, “It is lousy healthcare.”
Last month Senate Majority Leader Mitch McConnell, a Republican, said in an interview with Kentucky Educational Television that before the election, he assumed Trump did not have a chance of defeating Hillary Clinton and that Democrats would retake control of the Senate, ending any talk of repealing Obamacare.
But following Trump’s win and Republicans retaining their Senate majority, the Republicans find they have to deliver on their campaign promise, even though they have not agreed on a replacement healthcare program.
McConnell has said his top priorities for the new Congress were dealing with the “massive overregulation” he said had been a brake on the U.S. economy and making changes in the tax code to stop companies from moving jobs out of the country.
Republican lawmakers also want to curtail regulations aimed at controlling industrial emissions that contribute to climate change, and roll back banking industry reforms enacted after the near-collapse of Wall Street in 2008.
Republicans might use upcoming spending bills funding government agencies to try to kill some of those regulations. Trump also is expected to try to use his executive powers toward that end.
OBAMACARE DEFENSE
The first meeting of the 115th Congress will be full of ceremony, as the 435 members of the House of Representatives and a third of the 100-member Senate are sworn in.
Amid the celebration will be a move by House Republicans to clear the decks for Obamacare repeal.
That will come in the form of a vote on rules governing House procedures in the two-year term of the chamber. Tucked into the rules package is a move to prevent Democrats from slowing or stopping Obamacare repeal legislation because of the potential cost to the U.S. Treasury of doing so.
Leading Democrats warned of a fierce battle over Obamacare and said they planned to mobilize grassroots support for it. Obama is scheduled to meet on Wednesday with congressional Democrats to discuss strategies for fending off the Republican attacks on Obamacare.
Vice President-elect Mike Pence said he would meet on Capitol Hill on Wednesday with lawmakers about plans for replacing Obamacare and rolling back other regulations.
Trump’s Cabinet nominees were to begin meeting with senators on Tuesday ahead of Senate confirmation hearings.
The Senate also is expected to receive a Supreme Court nomination from Trump early in his term to replace conservative Justice Antonin Scalia, who died last February. Republicans refused to consider Obama’s nomination of Merrick Garland last year.
Prominent Republican Senator John McCain has warned that Rex Tillerson, Trump’s choice for secretary of state, will have to explain his relations with Russian President Vladimir Putin, who McCain has called a “thug and a murderer.”
Tillerson, who spent much of his career at Exxon Mobil Corp <XOM.N>, has been involved in business dealings in Russia and opposed U.S. sanctions against Moscow for its incursion into Crimea.
(Additional reporting by Steve Holland in Washington and Gina Cherulus in New York; Writing by Richard Cowan and Roberta Rampton; Editing by Chizu Nomiyama and Bill Trott)